|
||||||||||||||||||||
|
Thoracic Radiation
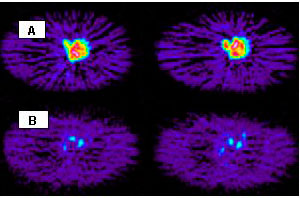
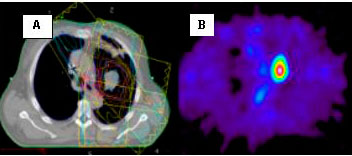
Oncology Service Thoracic Radiation Oncology Service at Massachusetts General Hospital has the following major research projects: (A) translational research, and (B) clinical research. A. Translational Research Translational research means a translation of promising imaging methods/treatments proven in basic science research into clinical research in humans. Molecular imaging is a new and promising method with which biochemical processes in cancer cells as well as living normal can be measured. All living cells have hexokinase, an enzyme essential for sugar metabolism. Cancer cells have this enzyme 6 to 10 times higher than the surrounding normal cells. Since cancer cells have such a high level of hexokinase activity, this difference in the level of hexokinase can be exploited in making a diagnosis and also monitoring tumor response to radiation or radiation and chemotherapy. The goals of the current research are: 2. Develop 3-dimensional isodose map for targeted intensity modulated (IM) RT or IM proton, 3. Develop 3-D molecular imaging map for targeted therapy using IM
RT, chemotherapy, biological agents aiming for cTCP ??95%.
B. Clinical Research Major clinical research includes:(1) Radiation dose escalation study,
(2) 4-dimensional RT planning, and (3) optimized radiation therapy according
to normal tissue tolerance.
Both basic science research and clinical research are closely related.
The findings from the basic science research are tested and verified
in the clinical research. The results of the translational research
are to be applied to:(1) Radiation dose escalation study, (2) 4-dimensional
RT planning, and (3) optimized radiation therapy according to normal
tissue tolerance.
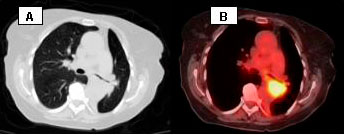
Conclusion Our study deals with quantitative correlation between FDG uptake measured with FDG PET 10-12 days after completion of radiation therapy and subsequent local tumor control at 12 months. From this correlation, we can determine the threshold value of FDG uptake below which local recurrence is less than 5%. Such threshold value of FDG uptake representing more than 95% of local tumor control at 12 months is a critical information for individualized and optimized radiation therapy in terms of radiation dose and target volume. There is a real promise that this research in molecular imaging will greatly help improve the results of the current treatment for lung Cancer. Noah C. Choi, M.D. Distinguished Scholar in Thoracic Oncology |
|||||||||||||||||||
| |
||||||||||||||||||||
| Home
| About Marcia | Facts
Page | Early Detection | How
You Can Help Upcoming Events | Contact us | Resources Design and layout by tgoburgess@hotmail.com W ebmaster afiasewaa@hotmail.com |
||||||||||||||||||||